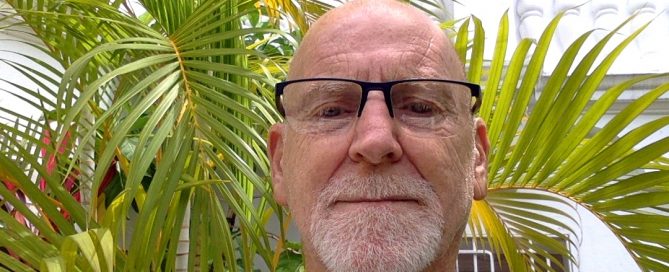
Adrian Fletcher (She/Her)
Hi, my name is Adrian Fletcher. I am a psychologist, trauma therapist, consultant, speaker, and writer. I live with both Complex Posttraumatic Stress Disorder and Dissociative Identity Disorder (DID) formally known as Multiple Personality Disorder. In 2017 after an attempt at my own life I spent time in a psychiatric hospital and residential treatment facility. [...]