I come from a family with a history of depression and anxiety. My dad and two of my brothers have bipolar disorder. My mom has an undiagnosed anxiety disorder. And I struggle with both mood and anxiety disorders. Because of this familiarity with mental illness, I played the helping role in my family for many years before I chose my profession. So becoming a clinical psychologist almost felt like a calling rather than a choice.
I first became depressed in high school. It’s hard to separate the angst of adolescence from clinical depression, but I had thoughts of suicide by the age of 15, so I’ll say that it started then. At that time, my diagnosis would have been dysthymic disorder—a more chronic, lower grade version of depression.
When I left for college at 18, I crossed over to major depression. However, I didn’t do anything about it for a year. At 19, I had my first therapy session with a psychiatrist who confirmed my diagnosis of depression. At the time, that was enough to make me feel better—to have someone tell me that what I was going through was real.
So I didn’t follow up with therapy until after I graduated from college, when I was 22. I can’t say I thought that therapist was particularly helpful. He never told me his opinion on anything, never gave me homework, never offered me another way to look at things.
The 3rd time I went to therapy was with my boyfriend right before we got engaged. I was 25 at the time. It was clear that she thought that our relationship problems were because of my depression and suggested that I go on meds, which really pissed me off. We didn’t see her for very long.
Still, she planted the seed of meds in my mind, and I started a trial of antidepressants about 6 years after she suggested it. And it did help. But after a year and half, I stopped taking them because I didn’t want to have to rely on meds to feel “normal.” Then I started them again a few years later when my husband and I started talking about separation.
I also went back to therapy. And she is the therapist who I have seen on and off for 13 years now. Her unconditional acceptance and belief in me, over time, has allowed me to accept and believe in myself. Still, I would see her for as little as I could get away with until I became functional, because I didn’t think I deserved to take up more of her time.
My 2nd major depressive episode happened almost 6 years ago when I was 40. I had stopped taking my meds again, and about 3 months later, I got depressed again. And it was even worse than the first time. It probably took me about 9 months to recover completely.
This time I was not able to just restart my meds and return to normal, so I saw a psychiatrist for the second time. Surprisingly, he was more concerned about things like light therapy, sleep hygiene, and supplements (Omega-3, NAC, Folic Acid) than he was about antidepressants. But I had to take those, too. He also added Ativan, because my anxiety had worsened, and Lamotrigine for bipolar depression, because of my family history and my hypomanic episodes.
It was difficult to accept that for the rest of my life I would be on a regimen that required an AM and PM pill box. But I had suffered so much through this last depressive episode that I got over it and was thankful to pharmaceutical companies for coming up with drugs that could make me feel like myself again.
Since that last depressive episode, I have gotten much better at taking care of myself. Mental health professionals have a tendency to put other people’s needs first, usually to their own detriment. I guess it’s sort of like how physicians make terrible patients. However, my determination to avoid a 3rd major depressive episode has motivated me to make my well-being a priority.
I have never shared this detailed of an account of my mental health history with anyone because I was ashamed of my depression. I felt like a failure. I was supposed to have everything under control, but sometimes I was struggling more than my clients were. But then a few years ago I decided to write a book about self-acceptance where I make use of both my personal and professional experience.
I decided to start with a mental health blog where I would be open and honest about all of the things that I ordinarily try to hide as a way to demonstrate how to practice self-acceptance. Because it’s that hard to do. Even when you know what you’re supposed to do.
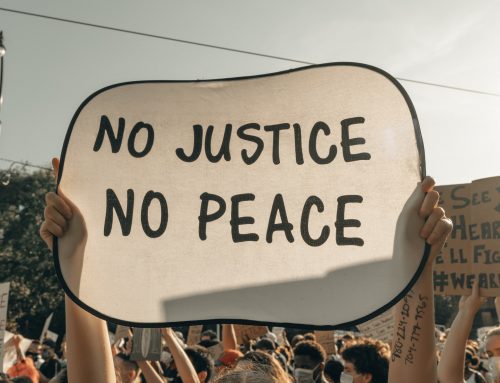
Surprisingly, readers are more interested in my personal experience than my expertise. Although I think it helps them to know that I am a psychologist, because it’s further proof that everyone struggles. Being an expert doesn’t make you exempt from suffering. From avoiding help. From resisting treatment. It is all a process that slowly improves with time. And as I blog and get feedback from readers, I become increasingly more comfortable with being me.
So even though I started this blog to help other people, it has turned out to be the best gift I have ever given to myself.
Christy is a clinical psychologist at the University Counseling Center at Washington and Lee University. Her areas of interests include women’s issues, diversity, and positive psychology.






*happy claps* this is wonderful to read. Since I came out of the mental illness as it were I feel grateful too for the ways in which it has helped me and helped others too, even if it just encourages them to read and learn. You are inspiring.
Thanks Helen!